Diagnosis of Papillary Thyroid Cancer
- There are approximately 64,000 new thyroid cancers diagnosed in the United States annually
- The diagnosis of papillary thyroid cancer accounts for approximately 85% of all thyroid cancers
- The diagnosis of papillary thyroid cancer is most common in women between the ages of 30 to 50
- The diagnosis of papillary thyroid cancer may occur at any age including infants, children and later years of life
- The diagnosis of papillary thyroid cancer effects women three times more frequently than it does men
- The diagnosis of papillary thyroid cancer is the fifth most common cancer affecting women in the United States
Diagnosis of Papillary Thyroid Cancer: How Is It Made?
The diagnosis of papillary thyroid cancer is usually a surprise to both the patient as well as the health care provider that discovers it. Identifying an expert in thyroid cancer surgery is the most important step! This is not a minor step. In fact, it is one of the most important tasks of a patient when they have received a diagnosis of papillary thyroid cancer. See what our patients say about us on our Google reviews and others including Health Grades and Rate MDs. See our reviews and 5 star ratings on Google.
When a patient, with a diagnosis of papillary thyroid cancer does present with symptoms, the most common symptom is a lump in the neck. Other symptoms which may occur with the diagnosis of papillary thyroid cancer may include changes in the quality of their voice, difficulty swallowing or breathing, and pain or tenderness in or around the neck or ear. More subtle symptoms of throat clearing and cough or an irritating feeling are sometimes seen. Any diagnosis of papillary thyroid cancer associated with change in voice, swallowing, breathing or pain are very serious symptoms and requires prompt and thorough evaluation. references include Tuttle RM, Ball DW, Byrd D, et al. Thyroid Carcinoma. J Natl Compr Canc Netw. 2010 Nov;8(11):1228-74. Changes in voice requires urgent evaluation and very expert thyroid surgery care.
Signs or symptoms might suggest that you have a diagnosis of papillary thyroid cancer, but you will need tests to confirm the diagnosis. The following are a list of tests that are frequently used in patients with a diagnosis of papillary thyroid cancer
- Complete Medical History and Physical Examination
- Ultrasound guided Fine Needle Aspiration (FNA)
- Genetic Testing only for an unclear diagnosis
- Scans and Xrays
- Ultrasound
- MRI Scan
- PET/CT Scan
- Blood Tests
- TSH
- T3 and T4
- Thyroglobulin (we obtain but not all doctors do so)
- Thyroglobulin Antibody (we obtain because it lets us know if there is an underlying inflammatory condition of the thyroid)
- Laryngoscopy (looking at the voice box)
Medical history and physical examination is required for all patients with a potential diagnosis of papillary thyroid cancer. If there is a suspicion that you may have a diagnosis of papillary thyroid cancer, your health care professional will want to know your complete medical history. You will be asked questions about your possible risk factors, symptoms, and any other health problems or concerns. If someone in your family has had a diagnosis of papillary thyroid cancer, this is an important factor. Your doctor will examine you to get more information about possible signs of thyroid cancer and other health problems. During the exam, the doctor will pay special attention to the size and firmness of your thyroid and any enlarged lymph nodes in your neck. Examination of your voice box is part of the physical examination obtained by the surgeon for any thyroid lump. This is called a laryngoscopy and more is written about it at the end of this section.
The Diagnosis of Papillary Thyroid Cancer is Made by Fine Needle Aspiration (FNA) Biopsy
- The diagnosis of papillary thyroid cancer is made with an ultrasound guided small sampling of cells from the thyroid gland or neck lymph nodes (or both in some instances).
- Ultrasound is used to see the thyroid or the lymph node(s) during the biopsy, which helps make sure they are getting FNA samples from the right areas.
- FNA is generally done on all thyroid nodules that are big enough to be felt. This means that they are larger than about 1 centimeter (about 1/2 inch) across.
- FNA biopsies of swollen or abnormal appearing lymph nodes in the neck may be more informative than the thyroid nodule itself in obtaining a diagnosis of papillary thyroid cancer.
- Cells from the suspicious area are removed without an incision or discomfort and looked at under a microscope.
- The process of obtaining this small sampling of cells is called fine needle aspiration (FNA) cytology.
- This type of biopsy can usually be done in your doctor’s office or clinic.
- Before the biopsy, local anesthesia (numbing medicine) may be injected into the skin over the thyroid nodule.
- Your doctor will place a thin, hollow needle directly into the nodule to aspirate (take out) some cells and possibly a few drops of fluid into a syringe.
- The doctor usually repeats this 2 or 3 more times, taking samples from several areas of the nodule.
- The content of the needle and syringe are then placed on a glass slide and then the FNA samples are then sent to a lab, where they are looked at under a microscope by the expert Cytologist to see if the cells look cancerous or benign.
- Cytology means looking at just the cells under the microscope.
- Thyroid cytology requires an expert physician (called a Cytologist) trained specifically in the diagnosis of papillary thyroid cancer!!!
- Unfortunately, the diagnosis of papillary thyroid cancer is frequently misinterpreted by unskilled or inexperienced Cytologists.
- Bleeding at the biopsy site is very rare except in people with bleeding disorders. Even when this occurs, the bleeding is almost always very self limited. Be sure to tell your doctor if you have problems with bleeding or are taking medicines that could affect bleeding, such as aspirin or blood thinners.
- Sometimes an FNA biopsy will need to be repeated because the samples didn’t contain enough cells.
- Most FNA biopsies will show that the thyroid nodule is benign.
- Rarely, the FNA biopsy may come back as benign even though a diagnosis of papillary thyroid cancer is actually present.
- Sometimes the test results first come back as “suspicious” for a diagnosis of papillary thyroid cancer. In such circumstances, the decision making should be in keeping with the management of a diagnosis of papillary thyroid cancer.
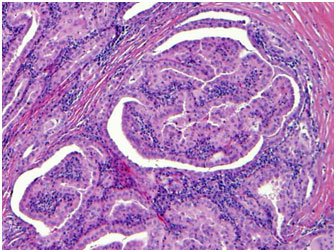
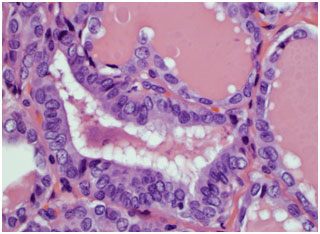
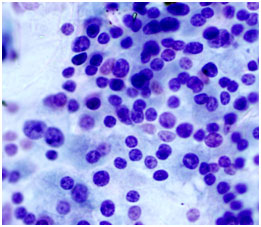 A cytology slide showing a good sampling of cells. The Cytologist sees some dark blue cells. This is the nucleus or center of the thyroid cell which contains the DNA of the cell. Some of the nucleus appears to be “clearing” compared to other cells. The specimen is suspicious for a diagnosis of papillary thyroid cancer.
A cytology slide showing a good sampling of cells. The Cytologist sees some dark blue cells. This is the nucleus or center of the thyroid cell which contains the DNA of the cell. Some of the nucleus appears to be “clearing” compared to other cells. The specimen is suspicious for a diagnosis of papillary thyroid cancer.
Diagnosis of Papillary Thyroid Cancer: What If The Diagnosis is Not Clear?
Sometimes FNA results come back as “atypical cells of undetermined significance” (called ACUS). This occurs when FNA findings don’t show for sure if the nodule is either benign or malignant. If this happens, the doctor may order tests on the sample to see if there are genetic abnormalities noted (changed). There are several commercially available tests that doctors can send the samples to determine the risk of the cells being cancerous. Before you consider one of these test, you should ask yourself “what information do I seek?” and “How will this information change my approach to my thyroid mass?”
For example, if you have a small thyroid nodule that is less than 1.5 cm and the FNA is atypical cell of undetermined significance and you prefer to monitor the nodule with ultrasound, then all of these tests may lead you to a surgery that you are already not desiring to pursue.
From an opposite standpoint, if you are above 5o years of age and have a 4cm thyroid nodule that has abnormal vascularity and on FNA is ACUS as well, then surgical excision would be recommended for multiple reasons including ultrasound appearance, size, and age. Genetic testing would only be beneficial in this circumstance if the surgeon and patient would propose a total thyroidectomy based upon this additional information. Importantly, before you proceed with a genetic test, make sure that this information is important to determining what your next step should or should not be. (Smith R, Ferris R. Utility of Diagnostic Molecular Markers for Evaluation of Indeterminate Thyroid Nodules. JAMA Otylaryngol Head Neck Surg. 2016)
The current commercially available genetic testing for thyroid nodules are Afirma, Asuragen, ThyGenX/ThyraMir and Thyroseq.
- The Veracyte test or Afirma Test has the best ability to tell whether the FNA cytology is benign. This is called a “rule out” test.
- Both Asuragen and Thyroseq3 are “rule in” tests. What this means is that they look for genetic abnormalities known to be associated with a diagnosis of papillary thyroid cancer. Finding these particular genetic changes makes a diagnosis of papillary thyroid cancer much more likely, and in some circumstances may also play a role in determining the best surgery for the cancer.
If the diagnosis of papillary thyroid cancer is not clear after an FNA biopsy, you might need a more involved biopsy to get a better microscopic examination of the nodule or thyroid mass. In particular, if the doctor has reason to think the nodule is suspicious for a diagnosis of papillary thyroid cancer based upon the nodule size, symptoms, or ultrasound appearance, the preferred biopsy is a thyroid lobectomy (removal of the half of the thyroid gland that possesses the nodule). Thyroid lobectomies are done in an operating room while you are under general anesthesia (in a deep sleep). A lobectomy can also be the main treatment for many patients with a diagnosis of papillary thyroid cancer.
However, FNA might not be the first test done if you have a suspicious lump in your neck. The doctor might order other tests first, such as blood tests and an ultrasound exam to get a better sense of whether you might have a diagnosis of papillary thyroid cancer. These tests are described following this section.
Imaging tests for a Diagnosis of Papillary Thyroid Cancer
Imaging tests may be done for a number of reasons, including to help find suspicious areas that might be cancer, to learn how far cancer may have spread, and to help determine the extent of surgery and the role of other treatments or therapies.
People who have or may have a diagnosis of papillary thyroid cancer will get one or more of the following tests:
Ultrasound
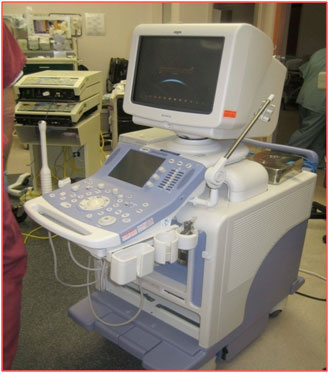 A high resolution ultrasound machine for evaluation of the thyroid and neck.
Ultrasound uses sound waves to create pictures inside your neck. The thyroid ultrasound must not only examine the thyroid gland but also must include a comprehensive examination of your neck lymph nodes. For this test, a small, wand-like instrument called a transducer is placed on the skin in front of your thyroid gland and all levels of the neck. It gives off sound waves and picks up the echoes as they bounce off the thyroid (and other underlying neck structures). The echoes are converted by a computer into a black and white image on a computer screen. You are not exposed to any radiation during this test. Dr. Clayman has also published about the importance of ultrasound in papillary thyroid cancer diagnosis. Thyroid 2012:22 (4) 347 In papillary thyroid cancer, preoperative central neck ultrasound detects only macroscopic surgical disease but negative findings predict excellent long term regional control and survival.
This test can help determine if a thyroid nodule is solid or filled with fluid. (Solid nodules are more likely to be cancerous.) It can also be used to check the number and size of thyroid nodules. Further, it can even reveal what the blood supply looks like to these nodules. How a nodule looks on ultrasound can sometimes suggest if it is likely to be a cancer, but ultrasound can’t tell for sure. Importantly, a cystic nodule is most commonly benign (not cancer). However, a cystic lymph node in the bottom half of the neck is most commonly a diagnosis of papillary thyroid cancer.
A high resolution ultrasound machine for evaluation of the thyroid and neck.
Ultrasound uses sound waves to create pictures inside your neck. The thyroid ultrasound must not only examine the thyroid gland but also must include a comprehensive examination of your neck lymph nodes. For this test, a small, wand-like instrument called a transducer is placed on the skin in front of your thyroid gland and all levels of the neck. It gives off sound waves and picks up the echoes as they bounce off the thyroid (and other underlying neck structures). The echoes are converted by a computer into a black and white image on a computer screen. You are not exposed to any radiation during this test. Dr. Clayman has also published about the importance of ultrasound in papillary thyroid cancer diagnosis. Thyroid 2012:22 (4) 347 In papillary thyroid cancer, preoperative central neck ultrasound detects only macroscopic surgical disease but negative findings predict excellent long term regional control and survival.
This test can help determine if a thyroid nodule is solid or filled with fluid. (Solid nodules are more likely to be cancerous.) It can also be used to check the number and size of thyroid nodules. Further, it can even reveal what the blood supply looks like to these nodules. How a nodule looks on ultrasound can sometimes suggest if it is likely to be a cancer, but ultrasound can’t tell for sure. Importantly, a cystic nodule is most commonly benign (not cancer). However, a cystic lymph node in the bottom half of the neck is most commonly a diagnosis of papillary thyroid cancer.
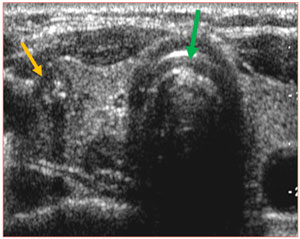 Ultrasound of the thyroid gland. The green arrow points to the breathing tube (trachea). The yellow arrow points to a nodule in the right side of the thyroid gland (the ultrasound pictures are a mirror image: meaning left side of image is on the patient’s right side and vice versa) which is a FNA biopsy proven diagnosis of papillary thyroid cancer.
Ultrasound of the thyroid gland. The green arrow points to the breathing tube (trachea). The yellow arrow points to a nodule in the right side of the thyroid gland (the ultrasound pictures are a mirror image: meaning left side of image is on the patient’s right side and vice versa) which is a FNA biopsy proven diagnosis of papillary thyroid cancer.
For thyroid nodules, ultrasound is used to guide a biopsy needle into the thyroid nodule to obtain a confident sampling of the cells within it.
Expert ultrasound can also help confirm a diagnosis of papillary thyroid cancer which has spread to the lymph nodes of the neck. The expert ultrasonographer will look for multiple changes. Although many unskilled observers would believe that size is a major issue, but it actually is not. High resolution ultrasound can detect a diagnosis of papillary thyroid cancer spread to lymph nodes as small as 1-2 mm (the size of a tip of a ball point pen). When looking at the lymph nodes in the neck with ultrasound, the following are important criteria which may lead to a FNA needle biopsy to confirm disease.
- Full of rounded lymph nodes
- Displacement or disruption of the normal ultrasonic “architecture” of a lymph node
- Cystic lymph nodes
- Microcalcifications within lymph nodes (small ultrasonic calcifications)
- Disorganized vascular flow to the lymph node
- Larger or asymmetric lymph nodes when comparing one side of the neck to the other
- Location, location, location-the diagnosis of papillary thyroid cancer spread to neck lymph nodes is quite predictable.
- Editorial note: One weakness of ultrasound is that it cannot distinguish cancerous from inflammatory lymph nodes. Both can have very similar appearances however ultrasound guided FNA will provide the necessary microscopic ability to confirm or rule out a diagnosis of papillary thyroid cancer.
- The quality of the ultrasound machine
- The device that is held in the hand of the technician (the transducer) producing the sound waves
- The experience and the skill of the ultrasound technician
- The experience of the radiologist or diagnostician who is interpreting the study.
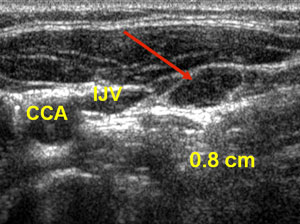 Ultrasound of the neck lymph nodes. CCA is the common carotid artery, IJV is the internal jugular vein. The red arrow points to an 8 mm lymph node which FNA confirms a diagnosis of papillary thyroid cancer spread (metastatic) to a lymph node.
Ultrasound of the neck lymph nodes. CCA is the common carotid artery, IJV is the internal jugular vein. The red arrow points to an 8 mm lymph node which FNA confirms a diagnosis of papillary thyroid cancer spread (metastatic) to a lymph node.
We perform an ultrasound on all of our patients ourselves because we have learned that ultrasounds performed elsewhere are not as accurate as we need. The most highly skilled ultrasound will detect abnormalities within lymph nodes within 1-2 mm. This is approximately the size of a ball point pen head. Your ultrasound should be performed by someone who is specifically dedicated to the ultrasound examination of the thyroid and neck. Experience means everything when you are considering the sensitivity of neck ultrasound.
The ultrasound study will critically look not only at the thyroid but all the tissues in your neck. The ultrasound can show whether something is cystic or solid. It can see the blood supply to a particular area. It can reveal microscopic calcifications that may indicate a cancer. Ultimately, your ultrasound will determine whether a biopsy with a tiny needle is indicated or whether simple blood test may only be indicated. Even if you have already had a biopsy, another biopsy may be indicated if:
- 1. The first biopsy did not provide a diagnosis
- 2. The ultrasound shows something that was previously not seen.
If ultrasound with needle biopsy detects that papillary thyroid cancer has spread to neck lymph nodes, other x-rays are indicated.
Computed tomography (CT) scan for Papillary Thyroid Cancer
The CT scan of the neck for papillary thyroid cancer is an x-ray test that produces detailed cross-sectional images of your body from the bottom of your brain to the middle of your chest. It can help determine the location and size of thyroid cancers, whether the cancer has invaded into any nearby structures, and whether they have spread to lymph nodes in nearby areas. A CT scan can also be used to look for spread into distant organs such as the lungs.
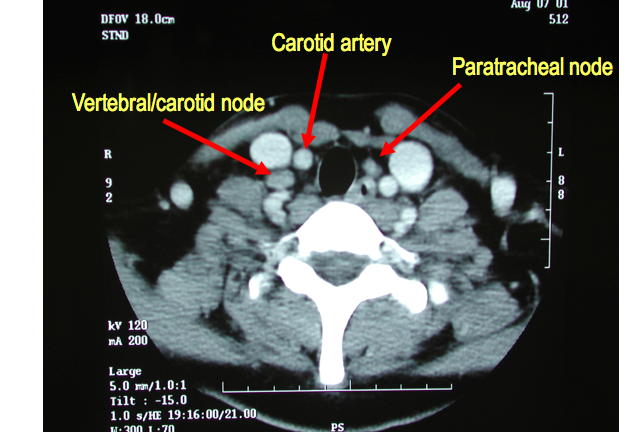 A CT scan (also called cat scan) of a patient with a diagnosis of papillary thyroid cancer. The CAT scan is a mirror image of the patient. Therefore objects on the left side of the Xray are actually on the right side of the body. This CAT scan shows very typical abnormal lymph nodes of papillary thyroid cancer. The lymph node seen on the left side of this Xray is called a carotid/vertebral lymph node. It is located between these two critically important blood vessels in our necks. The lymph node seen on the right side of the Xray is a lymph node of the central compartment of the neck. These are also commonly called paratracheal lymph nodes. These lymph nodes can be readily biopsied with ultrasound guided needle biopsy to confirm the papillary thyroid cancer spread to these lymph nodes.
A CT scan (also called cat scan) of a patient with a diagnosis of papillary thyroid cancer. The CAT scan is a mirror image of the patient. Therefore objects on the left side of the Xray are actually on the right side of the body. This CAT scan shows very typical abnormal lymph nodes of papillary thyroid cancer. The lymph node seen on the left side of this Xray is called a carotid/vertebral lymph node. It is located between these two critically important blood vessels in our necks. The lymph node seen on the right side of the Xray is a lymph node of the central compartment of the neck. These are also commonly called paratracheal lymph nodes. These lymph nodes can be readily biopsied with ultrasound guided needle biopsy to confirm the papillary thyroid cancer spread to these lymph nodes.
A CT scanner has been described as a large donut, with a narrow table in the middle opening. You will need to lie still on the table while the scan is being done. CT scans take longer than regular x-rays, and you might feel a bit confined by the ring while the pictures are being taken.
Instead of taking one picture, like a regular x-ray, a CT scanner takes many pictures while you lie on the table. A computer then combines these pictures into images of slices of the part of your body being studied. A CT scan designed for a diagnosis of papillary thyroid cancer is sliced at 1mm steps. It is an incredibly detailed study that creates very exquisite images.
Before the test, you will be asked to receive an IV (intravenous) line through which a contrast dye is delivered. This helps better outline structures in your body. The injection may cause some flushing (a feeling of warmth, especially in the face). Some people are allergic and get hives. Rarely, more serious reactions like trouble breathing or low blood pressure can occur. Be sure to tell the doctor if you have any allergies or have ever had a reaction to any contrast material used for x-rays.
You may have heard of a theoretical problem with using CT scans for a diagnosis of papillary thyroid cancer because the CT contrast dye contains iodine, which interferes with radioiodine scans. This should not be a consideration whatsoever. The iodine for the CT scan will be eliminated from the body in approximately two months. Therefore, at the most, there may just be a slight delay in the timing of radioactive iodine if this is thought to be potentially indicated in the management of the particular diagnosis of papillary thyroid cancer. The added information obtained from a CT scan may merely just delay the evaluation of radioactive iodine a month or so.
The CT scan for a diagnosis of papillary thyroid cancer provides different information to your doctor than the ultrasound. The ultrasound tells the doctor if there is something abnormal. The CT scan tells the doctor where the abnormality is located! Both studies complement each other. The CT scan of the neck also can look at areas of the neck that the ultrasound cannot study because sounds waves cannot pass effectively through bone, cartilage or air. Specifically, the CT scan can effectively see behind the jaw bone (mandible), collar bone (clavicle) or chest wall and also behind the voice box (larynx), breathing tube (trachea), and swallowing tube (esophagus). In all of these sites, the ultrasound examination can be quite limited, and therefore a CT scan may provide valuable additional information regarding where the papillary thyroid cancer is and where it is not. Ultimately, all of these studies will determine the extent of required surgery.
In patients with a diagnosis of papillary thyroid cancer above 55 years of age with advance disease in the thyroid gland itself or spread to lymph nodes, a CT scan of the chest should be obtained. The CT scan of the chest provides an excellent baseline examination (for following) of the lungs and the lymph nodes of the chest. Both of these sites are the highest risk of distant spread in patients with a diagnosis of papillary thyroid cancer.
Magnetic resonance imaging (MRI) scan
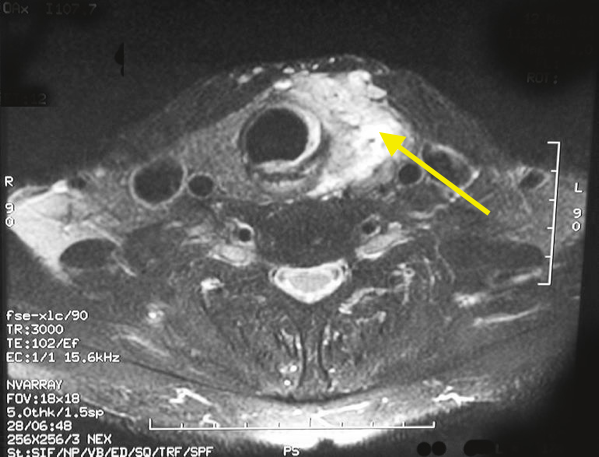 MRI of a papillary thyroid cancer of the left thyroid lobe. (MRI's show mirror images therefore what you see on the right is actually on the patient's left). The arrow points to the thyroid cancer which is more invasive and aggressive than the usual papillary thyroid cancer. This particular cancer has invaded through the natural covering of the thyroid gland into the overlying muscles as well.
MRI of a papillary thyroid cancer of the left thyroid lobe. (MRI's show mirror images therefore what you see on the right is actually on the patient's left). The arrow points to the thyroid cancer which is more invasive and aggressive than the usual papillary thyroid cancer. This particular cancer has invaded through the natural covering of the thyroid gland into the overlying muscles as well.
Like CT scans, MRI scans can be used to look for a diagnosis of papillary thyroid cancer in the thyroid, or cancer that has spread to nearby or distant parts of the body. But ultrasound is usually the first choice for looking at the thyroid and neck structures. MRI scans are particularly helpful in looking at the brain and spinal cord.
MRI scans use radio waves and strong magnets instead of x-rays, therefore there is no radiation exposure. The energy from the radio waves is absorbed and then released in a pattern formed by the type of body tissue and by certain diseases. A computer translates the pattern into a very detailed image of parts of the body. A contrast material called gadolinium is often injected into a vein before the scan to better show details.
MRI scans take longer than CT scans – often up to an hour. You may have to lie inside a narrow tube, which can upset people with a fear of enclosed spaces. Newer, more open MRI machines can sometimes be used instead. The machine also makes buzzing and clicking noises, so some centers provide earplugs or music to block this noise out.
MRI scans are very sensitive to movement and moving during the scanning process produces artifacts that make interpretation difficult. Because people are constantly swallowing and unconsciously moving their voice box and swallowing structures (and therefore their thyroid gland and surrounding lymph nodes, CT of the neck is our preferred cross sectional study of the neck in patients with a diagnosis of papillary thyroid cancer.
Positron emission tomography (PET)/CT scan
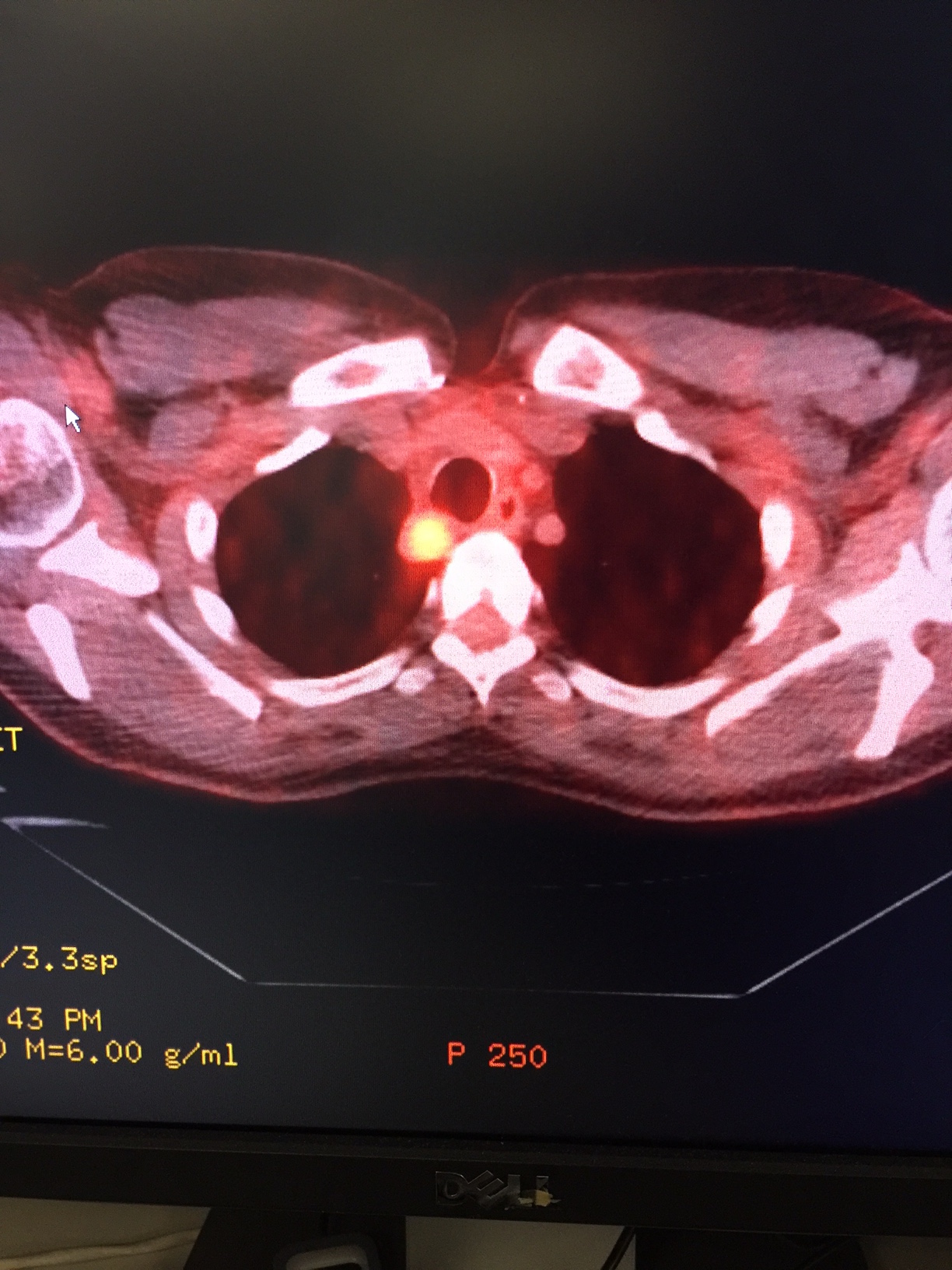 This is an example of a PET/CT scan of a patient with recurrent papillary thyroid cancer. The patient had already undergone three operations in the past. The bright orange circle on the left is a lymph node where the papillary thyroid cancer has spread. The black area to the left of the bright spot is the lungs. This metastatic lymph node with cancer is located in the area next to the trachea. This should only be removed by the most skilled surgeon. It will take about 15 minutes with a nearly 98% chance that it will never recur. I published these results in the Journal Thyroid. Long-term outcome of comprehensive central compartment dissection in patients with recurrent/persistent papillary thyroid carcinoma. Clayman GL, Agarwal G, Edeiken BS, Waguespack SG, Roberts DB, Sherman SI. Thyroid. 2011 Dec;21(12):1309-16.
This is an example of a PET/CT scan of a patient with recurrent papillary thyroid cancer. The patient had already undergone three operations in the past. The bright orange circle on the left is a lymph node where the papillary thyroid cancer has spread. The black area to the left of the bright spot is the lungs. This metastatic lymph node with cancer is located in the area next to the trachea. This should only be removed by the most skilled surgeon. It will take about 15 minutes with a nearly 98% chance that it will never recur. I published these results in the Journal Thyroid. Long-term outcome of comprehensive central compartment dissection in patients with recurrent/persistent papillary thyroid carcinoma. Clayman GL, Agarwal G, Edeiken BS, Waguespack SG, Roberts DB, Sherman SI. Thyroid. 2011 Dec;21(12):1309-16.
For a PET scan, a radioactive substance (usually a type of sugar related to glucose, known as FDG) is injected into the blood. The amount of radioactivity used is very low. Because cancer cells in the body generally utilize sugar as their energy source to grow, they absorb more of the sugar than normal cells. After waiting about an hour, you lie on a table in the PET scanner for about 30 minutes while a special camera creates a picture of areas of radioactivity in the body.
This test can be very useful if you have a diagnosis of papillary thyroid cancer that has:
- 1. Come back (recurred) following one or more surgeries
- 2. Diagnosis of papillary thyroid cancer that has spread to other sites in the body
- 3. Diagnosis of papillary thyroid cancer that doesn’t take up radioactive iodine (called non-iodine avid)
A PET/CT scan may be able to tell whether you have a diagnosis of papillary thyroid cancer which has spread to other sites of the body.
The PET/CT scan for a diagnosis of papillary thyroid cancer combines images of both a PET and CT scan at the same time. PET images alone are not very detailed. The computer shows the relative amount of radioactivity to a particular area and where the sugar is localized and it appears red or “hot”. The combination of these two images lets the doctor compare an abnormal area on the PET scan with its detailed appearance and location on the CT scan.
PET/CT scanning is not always positive in patients with a diagnosis of papillary thyroid cancer. If a patient has known papillary thyroid cancer and a PET/CT scan is obtained and does not reveal the cancer, generally speaking repeat analysis with PET/CT scan in the future is not warranted.
- Dedifferentiated or poorly differentiated papillary thyroid cancers (we have a whole section of pathologic subtypes of papillary thyroid cancers)
- A diagnosis of papillary thyroid cancer that no longer takes up radioactive iodine
- Recurrent Diagnosis of Papillary Thyroid Cancer (Cancers that have “come back” or recurred following one or more previous surgeries)
- A Diagnosis of Papillary Thyroid Cancer which has spread to sites outside of the neck (distant spread)
- A Diagnosis of Papillary Thyroid Cancer where the patient has a blood thyroglobulin level higher than anticipated for the disease that has been found
Blood Tests
Blood tests alone cannot tell the extent of a diagnosis of papillary thyroid cancer. Blood tests are a tool used with other studies, to monitor the adequacy of your thyroid hormone levels produced by your thyroid or by the intake of prescription thyroid hormones.
Thyroid cells and papillary thyroid cancers can also produce a protein called thyroglobulin which can be used as a blood monitoring tool in some patients.
(Importantly, some patients have an inflammatory condition of their thyroid called thyroiditis. The cause of this inflammation is called an autoimmune disease. This is the body reacting against itself. Some patients with autoimmune thyroiditis will produce an antibody to thyroglobulin. In those circumstances, analysis of thyroglobulin in monitoring a patient with a diagnosis of papillary thyroid cancer is quite limited since the antibody interferes with the blood analysis of thyroglobulin in these patients. Analysis and following the levels of antibody production is not indicative of papillary thyroid cancer, however some providers will monitor these levels as well.)
Thyroid-stimulating hormone (TSH)
Tests of blood levels of thyroid-stimulating hormone (TSH or thyrotropin) may be used to check the overall activity of your thyroid gland or how much thyroid hormone pill your body requires. Levels of TSH, which is made by a gland in the brain called the pituitary gland, may be high if you do not have enough thyroid hormone in your body. In previously untreated patients with a diagnosis of papillary thyroid cancer, their TSH level is usually normal. In patients with a diagnosis of papillary thyroid cancer that are being prepared for radioactive iodine treatment, they are most commonly taken off of thyroid hormone and their doctor will measure their TSH level which should be markedly elevated (radioiodine scans require the body to be hypothyroid). Alternatively, a medicine called Thyrogen (which is TSH produced as a drug) can also be given to patients with a diagnosis of papillary thyroid cancer by injection to make the body “appear” to be hypothyroid. After patients with a diagnosis of papillary thyroid cancer have undergone their surgery, their endocrinologist will likely want to keep their TSH level low to prevent stimulation of your thyroid gland and the potential stimulation of undetectable microscopic papillary thyroid cancer cells.
T3 and T4 (thyroid hormones)
These are the main hormones made by the thyroid gland. Levels of these hormones may also be measured to get a sense of overall thyroid gland function. The T3 and T4 levels are usually normal in patients with a previously untreated diagnosis of papillary thyroid cancer. Papillary thyroid cancer rarely produces either T3 or T4 hormones. Interestingly, even in patients with a diagnosis of papillary thyroid cancers that are quite massive with very little normal appearing thyroid tissue, hypothyroidism is quite infrequent as well.
Thyroglobulin
Thyroglobulin is a protein made by the thyroid gland that can be measured in blood sampling. Measuring the thyroglobulin level in the blood can’t be used to make a diagnosis of papillary thyroid cancer, but it can be helpful after treatment to determine whether the patient has (or does not) have disease. A common way to treat patients with a diagnosis of papillary thyroid cancer is to remove most or all of the thyroid gland by surgery and then use radioactive iodine to destroy any remaining thyroid cells. In patients with a diagnosis of papillary thyroid cancer, who have undergone total thyroidectomy with or without radioactive iodine treatment, their blood marker for thyroglobulin should be very low within several weeks of their surgery.
- There is still papillary thyroid cancer cells in the body
- There remains more thyroid tissue in the body which is producing thyroglobulin that has not been removed.
- There remains more thyroid tissue in the body which has not been destroyed by radioactive iodine treatment.
Importantly, in patients with a diagnosis of papillary thyroid cancer who have undergone total thyroidectomy, if the thyroglobulin level rises again after being low, it is a sign that the cancer has almost certainly recurred. Even thyroglobulin levels in the low detectable levels of less than 1 can be consistent with persistent papillary thyroid cancer.
Thyroglobulin Antibodies
Some patients have an inflammatory condition of their thyroid gland called thyroiditis. The most common cause of thyroiditis is a condition where the body produces an immune reaction to normal thyroid tissue. The body’s immune reaction is the production of an antibody and in autoimmune thyroiditis this can result in an antibody to the protein normally produced by thyroid cells called thyroglobulin. These thyroglobulin antibodies directly bind (grab onto thyroglobulin).
Very importantly, in patients with a diagnosis of papillary thyroid cancer who also have thyroiditis, their antibodies to thyroglobulin directly bind to thyroglobulin, and make the blood level of thyroglobulin appear to be zero (because the antibodies are clumped with the thyroglobulin protein and then not detected in the blood test).
Whenever the marker thyroglobulin is checked in the blood, the antibody to thyroglobulin must also be measured. If the antibody to thyroglobulin is detected, measuring thyroglobulin in the blood is not an effective marker in patients with a diagnosis of papillary thyroid cancer. Some providers will monitor thyroglobulin antibody levels and develop concerns when these antibody levels increase as well. Monitoring antibody levels is not an exact science and at times can be misleading in patients with a diagnosis of papillary thyroid cancer.
Other Blood Tests
You might have other blood tests as well. For example, if you are scheduled for papillary thyroid cancer surgery, tests will be done to check your blood cell counts, to look for bleeding disorders, and to check the function of your liver and kidneys.
Other Tests
Vocal cord exam (laryngoscopy)
Thyroid tumors can sometimes affect the function of your voice box. Even if your voice sounds normal to you and others, this does not mean that your vocal cords are functioning normally. If you are going to undergo a surgery for a diagnosis of papillary thyroid cancer, a procedure called a laryngoscopy will probably be done first to see if the vocal cords are moving normally. For this exam, the doctor looks through the nose or down the throat at the larynx (voice box) with a special thin tube with a light and a lens on the end for looking at the voice box. This special tiny scope is inserted through the nose and there is little to no discomfort associated with the examination. Alternatively, sometimes a mirror can be used to see the voice box as well.
For the Diagnosis of Papillary Thyroid Cancer: The Best Treatment is a Good Surgery!
The diagnosis of papillary thyroid cancer (carcinoma) is best treated almost exclusively by a good surgery. A good surgery is performed by a highly experienced surgeon. The best surgery provides a patient with a diagnosis of papillary thyroid cancer, which is the best opportunity for long term control and cure of their cancer. Following the diagnosis of papillary thyroid cancer, the optimal extent of initial surgery is determined by the ultrasound of the thyroid and neck to look closely at the thyroid gland and the lymph nodes of the neck. The section of ultrasound in the diagnosis of papillary thyroid cancer has a great general overview of the importance of high resolution ultrasound in the evaluation of papillary thyroid cancer. If the lymph nodes of the neck have some worrisome characteristics the next step is almost always a needle biopsy. If the diagnosis of papillary thyroid cancer involves the lymph nodes of the neck as well, another type of examination of the neck is needed. A CT scan of the neck with contrast is the preferred x-ray and should be obtained.
The diagnosis of papillary thyroid cancer in lymph nodes requires a surgery that will effectively remove the lymph nodes at risk of containing the papillary thyroid cancer. We have several pages on papillary thyroid cancer surgery, and one specifically on neck dissection for papillary thyroid cancer. If you have recently undergone a thyroid needle biopsy with a diagnosis of papillary thyroid cancer or have undergone a needle biopsy of a lymph node with a diagnosis of papillary thyroid cancer, these pages are for you.
Quick Facts!!!
- How the diagnosis of papillary thyroid cancer will behave is directly related to the size of the thyroid cancer within the gland itself.
- The diagnosis of papillary thyroid cancers that are less than 1.5 cm in size (less than ½ inch) have the best cure rates (nearly 100% for small papillary thyroid cancers in young patients). For this reason, the diagnosis of papillary thyroid cancer is sometimes referred to as “the good cancer”.
- The diagnosis of papillary thyroid cancer that develops in men that are above 55 years of age may be more difficult cancers to control in contrast to younger women.
- The diagnosis of papillary thyroid cancer may be associated with a history of radiation or x-ray exposure. Radiation exposure has the potential to be able to cause the development of papillary thyroid cancer. Most commonly, however, the diagnosis of papillary thyroid cancer occurs without any known risk factors.
- The diagnosis of papillary thyroid cancer is frequently associated with spread to lymph nodes of the neck, in up to in up to 50% of patients. For this reason, high definition ultrasound is required in all patients with suspected or confirmed diagnosis of papillary thyroid cancer. (Kouvaraki MA, Shapiro SE, et al. Role of preoperative ultrasonography in the surgical management of patients in thyroid cancer. Surgery. 2003. Dec;134(6):946-54.)
- The diagnosis of thyroid cancer is rarely associated with high thyroid function (hyperthyroidism) or low thyroid function (hypothyroidism).
The Diagnosis of Papillary Thyroid Cancer is Not Commonly Associated with Spread to Distant Areas Outside of the Neck (distant sites= distant metastases=spread to other parts of the body)
- The diagnosis of papillary thyroid cancer spread to distant sites of the body is uncommon.
- When it does spread to other areas of the body, the lungs and then bones are the most commonly found involved locations followed by the liver.
- The diagnosis of papillary thyroid cancer spread to distant sites is serious and requires an interdisciplinary thyroid cancer team that is very knowledgeable about the patient and the cancer itself.
- Distant spread of papillary thyroid cancer can make these cancers behave quite similar to other cancers that we all fear.
- The diagnosis of papillary thyroid cancer spread to distant sites significantly increases the risk of dying from this thyroid cancer.
- Importantly, despite the diagnosis of papillary thyroid cancer spread to distant sites, expert surgery remains a critical part of treatment in effectively controlling where the cancer began in the thyroid as well as spread to the neck lymph nodes.
- The diagnosis of papillary thyroid cancer with distant spread in the body is an indication for radioactive iodine treatment.
- Total thyroidectomy should be performed for the diagnosis of papillary thyroid cancer with distant spread, in most instances.
- The diagnosis of papillary thyroid cancer involving distant sites in the body is frequently associated with cancers that have spread to the neck lymph nodes. We have written several pages and also have videos so that you can understand how effective and well tolerated these comprehensive neck surgeries are in treating patients with thyroid cancer.
Diagnosis of Papillary Thyroid Cancers-Differing Pathologic Types
Conventional papillary thyroid cancer
- By far the most common pathologic diagnosis of papillary thyroid cancers
- Expert surgery is the mainstay of treatment
- High risk of spread to lymph nodes
- Readily diagnosed with fine needle aspiration (FNA) examination
- Risk of multiple areas in thyroid gland in 5-10 percent of patients
- The genetic defects associated with the diagnosis of papillary thyroid cancer are now well known to doctors and scientists.
- The most common genetic mutations associated are BRAF mutations and RET-PTC rearrangements.
Follicular variant of papillary thyroid cancer
- Very common pathologic type of diagnosis of papillary thyroid cancer
- Expert surgery is the mainstay of treatment
- Lymph node metastases common but less frequent than the conventional (or classic) type
- Microinvasive follicular variant of papillary thyroid cancer (now classified as equal to a non-cancerous lesion)
- May be difficult to diagnose with fine needle aspiration (FNA)
- Surgery frequently required to determine the diagnosis of follicular variant of papillary thyroid cancer
- Long term outcomes similar to conventional diagnosis of papillary thyroid cancer when this is invasive or spread to lymph nodes of the neck
Sclerosing variant of papillary thyroid cancer
- Almost appears scar like- that is how it got its name
- Can be a technically much more challenging surgery, but surgery is the foundation of treatment
- Nearly 100% incidence of lymph node spread in the neck
- Long term outcomes similar to conventional diagnosis of papillary thyroid cancer
Poorly differentiated (more aggressive variants and occur more commonly in the later decades of life)
- Some pathologic subtypes
- -Dedifferentiated variants
- -Tall cell, Columnar or Insular variants of papillary thyroid cancer
- -Hobnail papillary thyroid cancer
- Readily diagnosed from a fine needle aspiration biopsy of thyroid or lymph nodes
- Surgery is the primary treatment for this thyroid cancer whenever feasible
- Less commonly benefit from radioactive iodine treatment than the other types of papillary thyroid cancer
- The blood marker thyroglobulin (for the diagnosis of papillary thyroid cancer) may or may not be produced by these poorly differentiated thyroid cancers
- Genetic mutations are more common and more variable than the above mentioned more classical diagnosis of papillary thyroid cancers. These genetic mutations are usually multiple and may include TERT, p53, in combination with BRAF mutation. BRAF mutation, in and of itself is not an important genetic event.
- Special issues pertaining to poorly differentiated thyroid cancer
- -Can be more clinically aggressive than the more common diagnosis of papillary thyroid cancer (conventional and follicular variant of papillary thyroid cancer)
- -Spreads commonly to neck lymph nodes
- -Heightened risk of lung and bone distant spread than all other subtypes of diagnosis of papillary thyroid cancer.
The diagnosis of papillary thyroid cancer may also be associated with the following:
- A long standing history of a lumps or nodules in the thyroid gland
- A long standing history of thyroid goiter
- A history of radiation exposure or previous radiation treatment (other than routine x rays)
- A family history of papillary thyroid cancer
- Editorial note: The diagnosis of papillary thyroid cancer is not commonly associated with any risk factors. (For more information see section on Papillary Thyroid Cancer Genetics and Special Cases)