Medullary Thyroid Cancer Treatment
- What is the optimal treatment for this particular medullary thyroid cancer
- What are the patient's desires
- What are the capabilities and outcomes of the thyroid cancer team
Medullary Thyroid Cancer Surgery
Medullary thyroid cancer surgery is introduced here. The correct operation depends upon the medullary thyroid cancer extent of disease, patient evaluation, and surgeon's expertise. What is most important, is that all of the medullary thyroid cancer is removed from the neck in the initial surgery!!! That surgery does not necessarily have to be a large surgery (size of incision or length of time of surgery) but it needs to be a comprehensive surgery which removes all of the thyroid gland and all of the affected and high at risk lymph nodes of the neck. It can, however, also be a relatively small incision about 1.5 inches in length in the lower front of the neck.
Again, what the most critical issue is that all of the medullary thyroid cancer within the neck must be effectively removed at the initial surgery. An expert thyroid cancer surgeon is necessary to accomplish the correct surgery addressing all of the neck disease and maintaining all critical structures to maintain the patient's appearance, function, and quality of life. The wrong choice in surgeon increases the risk of medullary thyroid cancer persistence, recurrence, complications, and even ultimately survival of medullary thyroid cancer. Make sure you have a true medullary thyroid cancer surgery expert!!!
For medullary thyroid cancer, surgery by far, is the most common first treatment. In fact, in favorable smaller medullary thyroid cancers, surgery is not only the first treatment but is commonly the only treatment that may be indicated. It is critical that a highly experienced surgeon and the right surgery is obtained the first time. Medullary thyroid cancer surgery should only be done by expert surgeons.By choosing the right surgeon and surgery, you are provided the greatest opportunity for cure and long term control of disease. The wrong choice may lead to repeated surgeries, complications, and even worse!
Thyroid surgery was one of the first ever described surgeries in medicine, but early on it wasn't very pretty or safe. Over the past 100 years, thyroid surgery has evolved into its current state of the art by some of the most recognized names in surgical history. Today, in skilled hands, medullary thyroid cancer surgery may be considered an art form in and of itself.
Medullary thyroid cancer surgery must be considered in several different lights when you think about the neck. Surgery of the thyroid gland itself and surgery for the lymph nodes of the neck. The basic concept is however very simple, remove all of the cancer.
Total Thyroidectomy
In this surgery, the entire thyroid gland is removed. A small incision in the lower neck is required which is a little more than an inch in length unless the thyroid mass requires a longer length to allow it to be “delivered”. All of the critical structures on both sides of the thyroid are maintained including all four parathyroid glands and all four nerves that provide movement (recurrent laryngeal nerves) and sensation to the voice box (superior laryngeal nerves). A total thyroidectomy can be the most appropriate procedure in those individuals with a known RET mutation but without ultrasound evidence of medullary thyroid cancer or elevated calcitonin levels. In such circumstances, this is considered a prophylactic thyroidectomy. This can offer patients a life time cure of medullary thyroid cancer. The lymph nodes along the side and beneath the thyroid gland are also examined during this surgery to make sure that they are not cancerous as well.
Medullary Thyroid Cancer Surgery: Total Thyroidectomy with Central Compartment Lymph Nodes (the lymph nodes beneath and surrounding the thyroid gland, breathing tube (trachea) and swallowing tube (esophagus)
The removal of the lymph nodes of the central neck should routinely be performed initially when the thyroid gland is removed in the treatment of medullary thyroid cancer (see total thyroidectomy and central compartment dissection). If the medullary thyroid cancer should recur or persist due to an incomplete surgery, a secondary surgery of the central compartment may be required.
The central compartment lymph node surgery spares all critical structuresincluding the nerves to the voice box and all parathyroid glands not directly involved by cancer. Central compartment dissection extends from the carotid arteries on both sides of the neck, below to the blood vessels of the upper chest, and above to where the blood vessel of the upper portion of the thyroid gland begins off of the carotid artery (called the superior thyroid artery). [see a video of all the critical structures spared after a central compartment dissection]
- In medullary thyroid cancer, the central compartment lymph nodes are at risk of containing cancer in up to 70% of patients. That risk increases with the size of the medullary thyroid cancer. Even though the medullary thyroid cancer patient may have no identifiable lymph nodes with cancer on ultrasound or CT scan, complete dissection is indicated due the very high lymph node metastatic rate and recurrence rate without this intervention.
- In medullary thyroid cancer surgery, only expert surgeons who perform this surgery routinely are required to remove all the necessary structures and spare the nerves to the voice box and the critical glands that control calcium (parathyroid glands).
Extended or Complicated Thyroidectomy
Medullar thyroid cancer may sometimes be more aggressive than ultrasound or CT imaging suggested prior to undergoing surgery. In these cases, an expert surgeon that recognizes those "more aggressive" intraoperative findings such as growth or extension of the cancer outside of the thyroid gland or invasion of the cancer into adjacent structures such as the nerve to the voice box (recurrent laryngeal nerve), breathing tube (trachea), voice box, or esophagus-must adapt the surgery to adequately address the complete removal of the cancer. Unfortunately, occasional thyroid surgeons are commonly unprepared to perform the appropriate surgery and a subsequent surgery for persistent disease will be required (see the video of a complicated thyroidectomy). An incomplete first attempt at surgery greatly increases the risk for local recurrence, complications from subsequent surgeries, and even death from disease.
Medullary Thyroid Cancer Surgery For Spread of Cancer to Lymph Nodes Along The Side Of The Neck (anterolateral neck)
see a Modified Neck Dissection
- Just the presence of enlarged lymph nodes does not mean medullary thyroid cancer has spread and does not require additional surgery
- A procedure called an anterolateral neck dissection (or modified neck dissection), in untreated patients, should only be performed in instances of ultrasound with fine needle aspiration confirmed medullary thyroid cancer spread to lymph nodes in the side of the neck
- The medullary thyroid cancer anterolateral neck dissection is not the same neck dissection as for other cancers that occur in the neck. Medullary thyroid cancer spreads to particular areas of the neck called levels. Removing just some of the lymph nodes has been called “cherry picking” and is the wrong surgery! A medullary thyroid expert surgeon trained and experienced to perform modified neck dissections specifically for thyroid cancer is needed to prevent recurrent or persistent disease.
- The anterolateral neck dissection, in skilled hands, spares all critical nerves, muscles, and blood vessels which are not directly involved with cancer (very rarely are critical structures involved by papillary thyroid cancers). It is an approximately 40 minute surgery that removes lymph nodes and fatty tissue.
- The anterolateral neck dissection should be performed electively on the same side as large medullary thyroid cancer masses when the great vessels of the neck need to be dissected as well.
- Ultrasound and CT scan node negative necks need not be electively dissected with initial surgery for smaller medullary thyroid cancers.
Patient Presentation
A 32 year old firefighter, rescue public servant from Georgia presents with a suspicious right lateral neck lymph node. Fine needle biopsy suggests medullary thyroid cancer. He has no known family history of medullary thyroid cancer, adrenal tumors, or sudden cardiac death. Genetic testing reveals this to be a non-hereditary medullary thyroid cancer. His CT scans of his neck below reveal the suspicious right neck mass confirmed to be medullary thyroid cancer (arrow).
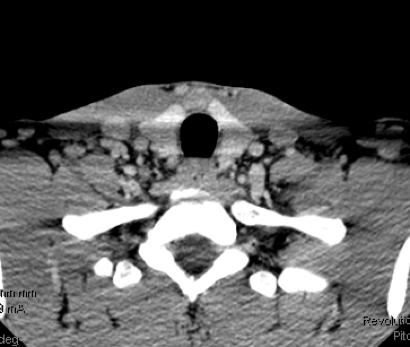
His CT scan of his chest and neck do not reveal evidence of spread. His calcitonin is 3179 and his CEA is 18.6 before surgery.

His surgery includes a total thyroidectomy, central compartment dissection and right anterolateral neck dissection. Right inferior parathyroid gland autotransplanted.
Pathology- Medullary thyroid cancer 1.4 cm
- Central compartment dissection 4 of 22 lymph nodes with spread of medullary thyroid cancer
- Right anterolateral neck dissection 6 of 36 lymph nodes with spread of medullary thyroid cancer
- Calcitonin below any detectable levels
- CEA 1.6 ng/ml
- Ultrasound without any abnormalities
Patient is highly likely cured of his medullary thyroid cancer.
Medullary Thyroid Cancer Surgery in Sites Other Than The Neck
Medullary thyroid cancer surgery is uncommonly proposed as a treatment approach when disease has spread to distant sites. Although surgery is not commonly proposed for distant spread of medullary thyroid cancer, consideration for surgery for distant disease is based upon the expert thyroid cancer team evaluation and considers the following issues:
- Where is the medullary thyroid cancer distant disease located?
- What are the risks and benefits of surgery?
- Are there other sites of distant spread?
- What medullary thyroid cancer treatments have already been used?
- What were the outcomes of other treatments for the medullary thyroid cancer?
- How fast is the medullary thyroid cancer growing?
- What are the patient's treatment desires?
- What are the other treatment options?
- What is the papillary thyroid cancer pathologic type (what do the cells look like under the microscope?
- What are the medullary thyroid cancer genetic mutations found?
Medullary Thyroid Cancer- Robotic Surgery Should Not Be Performed
Robotic surgery for the thyroid was developed largely in South Korea and brought to the United States several years ago as a “tool” in thyroid surgery. Its proposed benefits were to be the following:
- Absent or less noticeable neck incisions
- Improved visualization
- Less Surgeon Fatigue
Although we have been trained and performed robotic thyroid surgery, the following is the reality of robotic thyroid surgery:
- Incisions are tremendously longer but just not located on the front of the neck
- In medullary thyroid cancer, it is a one sided surgery approach to a both side of neck surgery!!!!
- The instruments used to perform the surgery are not as refined or delicate as the instruments used to perform the minimally invasive neck surgeries. (think of all the delicate structures that we have shown you here)
- Multiple surgeons are required
- The surgeon has no ability to “feel” in the neck. The fingers are the surgeon's third eye. Subtle changes in feel, hardness or extension of cancer can be totally unappreciated.
- It is not minimally invasive by any measure. It is maximally invasive but just at a distance from where the surgery is focusing.
- It is a much longer surgical procedure by any measure (the set up of the robot is longer than the average thyroid lobectomy).
- It is an inferior surgical approach to manage medullary thyroid cancer
- Unanticipated findings during surgery may not be able to be adequately addressed robotically.
Most importantly, the ability to perform a surgery is not an indication for a surgery! Robotic thyroid surgery is an inferior surgical approach in managing medullary thyroid cancer, any other type of thyroid cancer, or any thyroid lesion at risk of being a potential thyroid cancer.
Thyroid Hormone Suppressive Therapy is not beneficial in Medullary Thyroid Cancer
Thyroid hormone is a necessary hormone for life. The thyroid gland normally produces thyroid hormone to adequate levels. The amount of thyroid hormone produced by the body is strictly controlled by a portion of the brain called the pituitary gland. When the body has too little thyroid hormone, the pituitary gland senses the low levels and produces TSH (thyroid stimulating hormone). When thyroid hormone levels are elevated (too high), the pituitary does the opposite and lowers its production of TSH. This is called an endocrine feedback loop.
Most differentiated (papillary and follicular) thyroid cancer cells and all normal thyroid cells have a site on the surface of the cell that can stimulate their growth. This site is called a “receptor” and when stimulated by TSH (thyroid stimulating hormone) in normal thyroid cells it causes increased production of thyroid hormone. Medullary thyroid cancers are not derived from thyroid follicular cells. Medullary thyroid cancers are derived from the parafollicular (=around the follicular)C cells. These C cells do not possess the TSH receptor and therefore there is no known role for thyroid suppressive therapy in the treatment of medullary thyroid cancer. Medullary thyroid cancer patients should therefore have their thyroid hormone replaced at levels to maintain their TSH level at normal or near normal levels and equally maintaining their sense of well being. Lastly, it is also important that communication be open between your medullary thyroid cancer specialist and those that are caring for your primary care needs.
External Beam Radiation Therapy for Medullary Thyroid Cancer
Medullary thyroid cancer treatment with external beam radiation therapy is not commonly required or indicated. The planning and implementation of radiation therapy is beyond the goals for this website. However certain principles must be emphasized. Radiation therapy is not a substitute for incomplete surgery. What is meant by that is all the medullary thyroid cancer in the neck must be completely and effectively removed. Whenever feasible, medullary thyroid cancer patients should be reduced down to microscopic remaining neck disease, at most, also sparing voice box and swallowing tube function. Radiation therapy should not be given as a substitute for incomplete surgery. As a general rule, choosing to treat a medullary thyroid cancer with external beam radiation is a commitment that the surgeon believes that no meaningful re-operation will be feasible in the future and therefore radiation therapy is required to help control the medullary thyroid cancer (microscopic disease) remaining in the neck. In these circumstances, external beam radiation therapy is quite effective. Medullary thyroid cancer radiation therapy is also associated with significant short term and long term complications and effects that should not be taken lightly.
- Invade (grow into) the voice box (larynx), breathing tube (trachea) or swallowing tube (esophagus)
- Directly grow into the skin or deep structures in the neck
- Invade the tissues underneath the breast bone (sternum)
- are deemed unable to undergo another surgery if their cancer should return.
- Have spread to the spinal column and risk the spinal cord itself
- Have spread to the brain
- Have spread to bone and are causing pain or growth would place the bone at risk for fracture.
Medullary Thyroid Cancer Treatment for Persistent or Recurrent Disease:
Medullary thyroid cancer treatment for recurrences (cancer that has come back) or persistence (cancer that remains after initial therapy) depends mainly on where the cancer is, although other factors may be important as well. The recurrence may be found by either calcitonin and CEA blood tests or imaging studies such as ultrasounds, CAT scan or PET imaging.
If there is concern that the medullary thyroid cancer has come back in the neck, an ultrasound-guided biopsy is first done to confirm that it is really cancer. Medullary thyroid cancers are relatively easy to diagnose on FNA for recurrent disease. Cells obtained from FNA can be specially stained with a type of probe for calcitonin that gets stuck on that protein and can be seen microscopically. Additionally, FNA's can also be analyzed for calcitonin levels which will be markedly elevated if the mass if a recurrent medullary thyroid cancer.
Then, if the medullary thyroid cancer appears to be resectable (removable), surgery is often used. The extent of surgery would depend upon the location or locations of the persistent or recurrent follicular thyroid cancer and the prior surgeries and quality of surgeries that the patient has undergone. The sections of complicated thyroidectomy, central compartment surgery, and lateral neck dissection have been written for you and are appropriate for persistence or recurrent medullary thyroid cancer in any of these locations. We have examples of surgeries for just these types of circumstances for you to watch. Medullary thyroid cancer surgery for recurrent or persistent disease very effectively manages neck disease, sparing function and cosmetic appearance but should only be performed by very high volume and experienced medullary thyroid cancer surgeons. We have established our ability to control recurrent medullary thyroid cancer recurrences or persistence in the neck approaching 98% when the medullary thyroid cancer recurs in the thyroid location (central neck) or lateral neck (side of the neck).
Persistent or recurrent medullary thyroid cancer in residual thyroid tissue is much more concerning for the potential for the cancer to extend directly into the breathing tube or voice box. Only the most skilled and experience thyroid cancer surgeons should manage such circumstances. The purpose of this specific medullary thyroid cancer surgery is to maintain vocal and swallowing function, parathyroid function, and airway control. These are the most complicated and complex of all thyroid surgeries.
Targeted Therapy and/or Chemotherapy
For medullary thyroid cancer patients who have spread of their cancer to several places outside of the neck area or areas of disease within the neck that thyroid cancer surgery experts believe surgery could be more troublesome than the cancer itself, new therapies have been developed and approved by the FDA (Food and Drug Administration). Although these FDA approved medullary thyroid cancer targeted medications have been shown to be effective, none of these treatments are curative. Skilled physicians in prescribing these medications are required because of the necessity for close monitoring of symptoms, toxicities, and monitoring of the patient's medullary thyroid cancer.
The first FDA approved targeted therapy for medullary thyroid cancer was Vandetanib. The second approved targeted therapy for medullary thyroid cancer was Cabozantinib. Neither of these two drugs has been shown, yet, to prolong the lives of medullary thyroid cancer patients however both drugs are approved and have established clinical activity. Complications are common with these targeted therapies including diarrhea, nausea, high blood pressure, weight loss and more. Close clinical observation is required when medullary thyroid cancer patients are managed with systemic targeted therapy. Experts in medical endocrine oncology are those thyroid cancer team specialists that manage these medullary thyroid cancer patients. Again, these medications cannot be taken indefinitely and do not cure the medullary thyroid cancer patients.
Medullary thyroid cancer chemotherapy is rarely indicated. Experimental therapies such as new targeted therapies, immune therapy based treatments, and other novel approaches for medullary thyroid cancer patients should be developed in institutions directed and capable of performing such investigational studies.