Pediatric Thyroid Cancer: Why Choosing the Right Surgeon Matters More Than Ever

Pediatric Thyroid Cancer: Why Choosing the Right Surgeon Matters More Than Ever
Hearing that your child has cancer is every parent’s worst nightmare. And while thyroid cancer in children is rare, it’s the most common endocrine cancer in the pediatric population.
As a parent, you want the best care possible. But what does that look like when your child has thyroid cancer?
At the Clayman Thyroid Center, we specialize in thyroid surgery for patients of all ages. We operate on children and teenagers with thyroid cancer nearly every week, many of whom travel from across the country for expert surgical care.
In this article, I’ll walk you through what parents need to know about pediatric thyroid cancer, how it’s treated, and why choosing a high-volume thyroid surgeon, not a general pediatric surgeon, is the most important decision you can make for your child’s health.

Figure 1: A 13-year-old elite soccer player from Virginia faced an unexpected diagnosis of papillary thyroid cancer, but thanks to early detection, expert surgical care from Dr. Rashmi Roy, and a seamless operative plan, she's now on the road to recovery and ready to return to the sport she loves.
What Is Pediatric Thyroid Cancer?
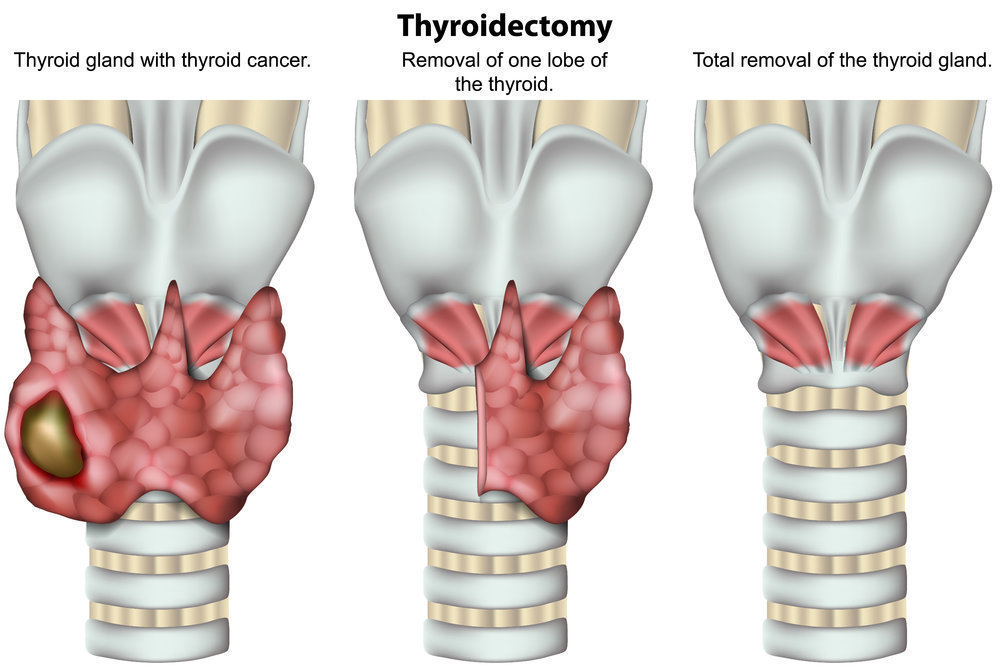
Thyroid cancer occurs when abnormal cells grow in the thyroid gland, a small butterfly-shaped organ located in the front of the neck. This gland produces hormones that regulate metabolism, growth, and development, so it plays a vital role in a child’s health.
Although thyroid cancer is much more common in adults, its incidence in children and teens is increasing. The most common type is papillary thyroid cancer, which accounts for over 90% of cases in kids. The next most common is follicular thyroid cancer. Together, these are referred to as differentiated thyroid cancers, and they tend to grow slowly but can spread to lymph nodes and sometimes even to the lungs.
Pediatric thyroid cancers tend to involve lymph nodes more commonly than adult thyroid cancers. That is why you need to see an expert thyroid surgeon who can perform an expert evaluation to determine the extent of surgery that the child needs. You want the child’s first surgery to be their last surgery.
What Causes Thyroid Cancer in Children?
In most cases, we don’t know exactly what causes thyroid cancer in kids. However, known risk factors include:
- Radiation exposure (especially to the head or neck)
- Family history of thyroid cancer
- Certain genetic syndromes
- Female gender (girls are 3 to 4 times more likely than boys to develop thyroid cancer)
Most children, however, have no identifiable risk factors. That’s why it’s so important to know the warning signs.
Signs and Symptoms: What to Look For
Thyroid cancer in children often goes unnoticed until a lump is discovered in the neck—either by a parent, a pediatrician, or even during a routine scan done for another reason. Symptoms may include:
- A lump or swelling in the neck
- Difficulty swallowing
- Hoarseness or voice changes
- Enlarged lymph nodes
In many cases, there are no symptoms at all—just a visible or palpable lump. If you notice anything unusual in your child’s neck, ask your pediatrician to order a neck ultrasound, the most accurate and non-invasive way to assess the thyroid gland.
How Is It Diagnosed?
Diagnosing thyroid cancer typically involves:
- High-resolution ultrasound of the thyroid and lymph nodes in the neck
- Fine Needle Aspiration (FNA) biopsy if the nodule has suspicious features, or if a lymph node has suspicious features
- Thyroid blood tests to assess gland function
Once thyroid cancer is diagnosed or strongly suspected, the next—and most important—step is surgery.
Surgery Is the Only Definitive Cure
Let’s be very clear: surgery is the only cure for thyroid cancer. No pill, no chemotherapy, no radiation therapy can eliminate thyroid cancer without removing the tumor, and the thyroid gland from which it grows.
Every child deserves a curative surgery done right the first time. That means removing either a portion of the thyroid gland or the entire thyroid gland, as well as any lymph nodes that are involved or at high risk for harboring cancer.
Done correctly the first time, surgery offers an excellent prognosis and cure rate for nearly every child.
Should You Choose a Pediatric Surgeon or a Thyroid Surgeon?
This is one of the most common—and most critical—questions parents ask.
Pediatric surgeons are incredibly skilled and compassionate physicians. But most pediatric surgeons are generalists—they perform surgeries across all organ systems in children, from appendectomies to hernia repairs. They might do a few thyroid surgeries per year, if that.
Thyroid cancer, on the other hand, demands subspecialty expertise.
The thyroid gland is surrounded by delicate, vital structures, including:
- The recurrent laryngeal nerves, which control the vocal cords
- The parathyroid glands, which regulate calcium in the blood
- Major blood vessels and the trachea
Preserving these structures—while ensuring complete cancer removal—requires precise, expert-level surgery. The risks of permanent voice damage, low calcium (hypoparathyroidism), or incomplete cancer removal are much higher in inexperienced hands.
That’s why children with thyroid cancer should be treated by an expert thyroid surgeon, not a pediatric surgeon. The surgeon’s experience with thyroid surgery matters far more than their patient’s age.
At the Clayman Thyroid Center, our surgeons perform more thyroid surgeries than any other center in the United States. We’ve performed over 2,500 thyroid cancer surgeries annually, including a high volume of pediatric cases.
What Happens After Surgery?
After a thyroidectomy, your child will:
- If necessary, start thyroid hormone replacement therapy, a daily pill that mimics natural thyroid hormone and ensures normal growth and development.
- Undergo regular follow-up appointments, including bloodwork and neck ultrasounds
Most kids recover quickly after surgery and return to normal activities within a week or two. Many go back to school within days. Full activity in sports and strenuous activity would be delayed for 3 weeks.
What’s the Long-Term Outlook?
The prognosis for children with differentiated thyroid cancer is excellent:
- Over 99% cure rate when treated with expert surgery
- Very low recurrence rates when the initial surgery is done correctly
- Normal life expectancy and full quality of life after treatment
The biggest threats to a great outcome are:
- Delayed diagnosis
- Incomplete or inadequate surgery
- Surgeons without thyroid-specific expertise
That’s why choosing the right surgical team upfront is so critical.
Why Families Travel to Us
Many of our pediatric patients travel from across the U.S. and around the globe because they want the best. We make the process as smooth and stress-free as possible for families, offering:
- Same-day evaluations, imaging, and surgery in most cases
- Concealed incisions that may fade away completely
- On-site ultrasound and pathology
- A warm, family-centered care environment
If your child has been diagnosed with thyroid cancer—or even if you're just concerned about a thyroid nodule—don’t wait. Contact us for a consultation. We’ll help you get the answers you need and the care your child deserves.
Final Thoughts from Dr. Roy
As a surgeon—and as a mother myself—I understand the fear and uncertainty that come when something is wrong with your child. When your child needs surgery, especially for cancer, it can feel overwhelming. But I want you to know there is a cure, and we will get there together.
Pediatric thyroid cancer, when treated with expert surgery, has one of the best survival rates of any childhood cancer. With the right care, your child can go on to live a completely normal, healthy, long life. I will care for your child the same way I would care for my own—because I know how much this matters.
If you have questions or need a second opinion, please don’t hesitate to reach out. We’re here to help.
Additional Resources
- Become our patient by filling out the form at this link.
- Learn more about The Clayman Thyroid Center here.
- Learn more about our sister surgeons at the Scarless Thyroid Surgery Center, Norman Parathyroid Center, and Carling Adrenal Center
- Learn more about the Hospital for Endocrine Surgery.