Change in Thyroid Nodule: Why You Should Know

Change in Thyroid Nodule: Why You Should Know
We often hear from patients concerned by changes in their thyroid nodules—whether it grew, characteristics on ultrasound changed, the nodule started to cause symptoms, or new nodules were diagnosed. In this blog, I will walk through different scenarios involving a change in a thyroid nodule, explain what the change could mean, and outline when a change warrants further investigation or procedural intervention.
1. Change in Thyroid Nodule Size: Slow Growth vs Rapid Expansion
A common trigger for anxiety is when a thyroid nodule increases in size. Most nodules, even benign ones, exhibit slow growth over months to years. Ultrasound surveillance at 12-month intervals can eventually reveal gradual enlargement—although this is typically not alarming.
- Slow growth (< 20% increase in volume/year)
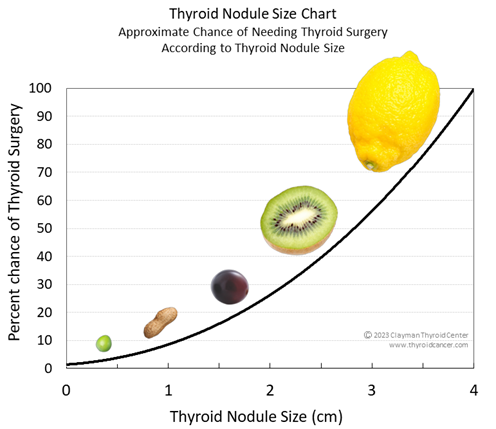
This represents expected biological behavior. We continue observation and ensure the change in thyroid nodule doesn’t meet any threshold for intervention. - Rapid growth or nodules ≥ 4 cm
Per our thyroid nodule size chart, nodules around 4 cm almost always require surgery due to symptoms, cosmetic concerns, size, and slight biopsy variability due to large volume. A sudden or noticeable increase in the size of a thyroid nodule over a short period of time is considered a red flag. While most benign nodules grow slowly and predictably, rapid growth can sometimes signal a more aggressive thyroid cancer.
When to be concerned?
- Rapid size increase in 12 months or less
- Nodule reaches ≥ 4 cm
- Symptoms such as difficulty swallowing, breathing, or a visible neck bulge occur
In these cases, further imaging, needle biopsy, and often surgical intervention are required.
2. Change in Thyroid Nodule Appearance on Ultrasound
Expert, high-resolution ultrasound offers more than size—it reveals nodule features tied to malignancy risk. A worrisome change in thyroid nodule may be seen in:
- New hypoechogenicity (darker appearance)
- Development of irregular borders, tiny or punctate calcifications (microcalcifications), or increased blood flow
- Shift from spongiform or cystic (usually benign) to a nodule with more suspicious features
A shift toward hypoechoic texture raises cancer concern. Hypoechoic nodules have higher malignancy rates and often merit surgical evaluation. Similarly, a spongiform nodule that loses its benign texture also becomes suspect. Nodules with microcalcifications or increased vascularity are also concerning and warrant further evaluation. In summary, even without significant size change, an evolving ultrasound appearance can prompt new biopsy or surgical consideration.
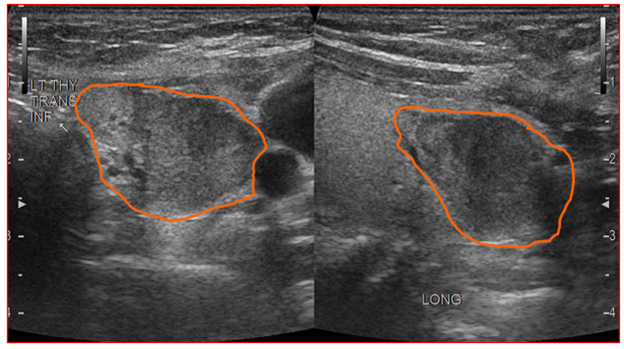
Figure 1: Hypoechoic left thyroid nodule. This was diagnosed as papillary thyroid cancer after surgical removal.
3. Change in Thyroid Nodule Cellular Status (Biopsy Results)
If a nodule is monitored, it may undergo Fine Needle Aspiration (FNA) if something changes. Thyroid nodule biopsies are classified and risk-stratified according to the Bethesda System for Reporting Thyroid Cytopathology (aka the Thyroid Bethesda System). Here’s what the different categories mean:
Bethesda I (Non-diagnostic)
Not enough cells were obtained during the needle biopsy to yield a diagnosis. The risk of cancer is still low (5-20%), but repeat FNA biopsy in 3-6 months can be done
Bethesda II (Benign)
Minimal cancer risk (2–7%). Continue surveillance unless other changes occur.
Bethesda III (Atypia of Uncertain Significance)
Cancer risk 12–30%. A repeat FNA, additional molecular testing, or surgery is appropriate.
Bethesda IV (Follicular Neoplasm)
Cancer risk is 23-34%. Additional molecular testing or surgery is indicated.
Bethesda V (Suspicious for Malignancy)
Cancer risk is 67-83%. Surgical management is indicated.
Bethesda VI (Malignant)
Cancer risk is 97-100%. Work-up for metastasis to the central and lateral compartments is indicated. This is followed by surgery.
2023 Bethesda System for Reporting Thyroid Cytopathology
|
Diagnostic category |
ROM average% (range) |
Usual management |
|
Bethesda I Nondiagnostic |
13 (5–20) |
Repeat with ultrasound guidance |
|
Bethesda II Benign |
4 (2–7) |
Clinical and sonographic follow-up |
|
Bethesda III Atypia of Undetermined Significance |
22 (12–30) |
Repeat FNA, molecular testing, diagnostic lobectomy, or surveillance |
|
Bethesda IV Follicular neoplasm |
30 (23–34) |
Molecular testing, diagnostic lobectomy |
|
Bethesda V Suspicious for Malignancy |
74 (67–83) |
Molecular testing, lobectomy, or near-total thyroidectomy |
|
Bethesda VI Malignant |
97 (97–100) |
Lobectomy or near-total thyroidectomy |
*Adapted from Ali SZ, VanderLaan P. The Bethesda System for Reporting Thyroid Cytopathology. 3rd ed. New York: Springer; 2023 (In Press).
Biopsy-identified malignancy typically leads to surgical removal of half or all of the thyroid.
A change in thyroid nodule cytology from benign to one of these categories is a significant red flag that requires expert evaluation and management.
4. Change in Symptoms: Pressure, Voice, or Hormonal Shifts
Sometimes a nodule begins to produce symptoms, indicating a change in thyroid nodule behavior:
- Compressive symptoms: A growing nodular mass may press on the trachea or esophagus, causing difficulty swallowing or breathing. A visible lump in the neck, pressure, and/or globus sensation (feeling of something stuck in the throat or “lump in the throat”) also can be the result of a growing or large nodule.
- Vocal changes: hoarseness, voice fatigue, or vocal cord weakness may reflect nerve involvement and warrant immediate evaluation.
- Hormonal activity: Rarely, nodules become “hot”/toxic and lead to hyperthyroidism. This is diagnosed with thyroid labs sometimes combined with a special nuclear medicine thyroid scan. These nodules generally have low malignancy risk but require treatment, whether that is surgery or radiofrequency ablation (RFA).
When to be concerned?
- New-onset neck fullness, pressure, or difficulty swallowing or breathing
- Hoarseness or vocal changes
- Biochemical evidence of thyroid hormone overproduction
Compressive symptoms or hormone activity may necessitate surgical or ablation therapies even if cancer risk is low.
5. Multiple Nodules or Changing Nodule Features
Multiple nodules complicate management. More nodules are harder to monitor. A change in thyroid nodules in this context, especially when nodules crowd each other—an obscure growth or raise overall concern. Furthermore, when multiple nodules are present, change in more than 1 nodule makes biopsy, RFA, and surgery more likely to be necessary.
- Multinodular goiter with enlarging nodules may lead to symptoms or cosmetic issues.
- Monitoring many nodules with numerous needle biopsies (more than 2-3) impractical; surgery is often recommended when ≥ 3 nodules show change, enlarge significantly, or cause symptoms.
When Change in a Thyroid Nodule Is Less Concerning
Not every change in a nodule is alarming.
- Slow growth in a benign Bethesda II nodule- Continued regular surveillance is most often recommended.
- Small nodules (< 1 cm) with mild changes or growth and no concerning ultrasound features are almost always low risk.
- Stable, benign-appearing nodules (cystic/spongiform, smooth borders, wider than tall, no microcalcifications, no hypervascularity) mean low cancer risk even with minor size fluctuations.
Key Takeaways on “Change in Thyroid Nodule”
|
Scenario |
How to Recognize a Change |
What It Might Mean |
Next Steps |
|
Slow growth (<20%/year) |
Ultrasound shows gradual increase |
Likely benign |
Continue annual ultrasound |
|
Rapid growth or ≥4 cm |
Nodule enlarges quickly or exceeds threshold |
Risk of symptoms/cancer |
Ultrasound + biopsy and/or surgery |
|
Ultrasound appearance worsens |
Hypoechoic, irregular borders, microcalcifications, etc. |
Higher malignancy risk |
New FNA / consider surgery |
|
Change in biopsy (Bethesda ≥III) |
Cytology category increases |
Elevated cancer risk |
Consider molecular testing +/- surgery |
|
New symptoms appear |
Pressure, hoarseness, swallowing difficulty |
Possible compressive or invasive changes |
Clinical evaluation, imaging, +/- surgery |
|
Multiple nodules evolve |
Several nodules grow or cause symptoms |
Goiter or multiple suspicious nodules |
Consider surgery, especially with symptoms |
What We Recommend
- Ultrasound surveillance is the cornerstone for monitoring changes in thyroid nodules. Small, benign-appearing nodules can be observed safely at 12- month intervals. Long-term, if the nodules are stable, they can be monitored even less frequently.
- Fine Needle Aspiration is indicated when nodules have suspicious traits, increase in size significantly, or show other noticeable changes on ultrasound. Even small nodules (1 cm or less) warrant a biopsy if the ultrasonographic appearance is suspicious enough.
- Surgical removal is recommended for malignant/suspicious biopsies, nodules ≥4 cm, or nodules causing compressive symptoms. RFA is an option for benign, symptomatic nodules, hot/toxic nodules, or benign nodules that are enlarging.
- Expert evaluation in a high-volume center is essential—both ultrasound and biopsy accuracy improve outcomes significantly.
If you’ve noticed a change in a thyroid nodule, bring it to your physician’s attention. The Clayman Thyroid Center is here to guide you with advanced ultrasound, precision biopsy, and thoughtful, personalized management.
Additional Resources
- Become our patient by filling out the form at this link.
- Learn more about The Clayman Thyroid Center here.
- Learn more about our sister surgeons at the Norman Parathyroid Center, and Carling Adrenal Center
- Learn more about the Hospital for Endocrine Surgery.